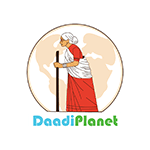
Skin pigmentation disorders affect millions of people worldwide, with melasma being one of the most common and challenging conditions to treat. Often called the “mask of pregnancy” or “chloasma,” melasma creates distinctive brown or gray patches on the face, leaving many feeling self-conscious and searching for effective solutions. This comprehensive guide explores the intricate world of skin pigmentation, delves deep into melasma’s causes and triggers, examines various treatment approaches, and introduces time-tested natural remedies that have helped restore skin confidence for generations.

The Science Behind Skin Pigmentation
Understanding melasma begins with comprehending how our skin produces color. Melanin, the pigment responsible for skin, hair, and eye color, is produced by specialized cells called melanocytes located in the basal layer of the epidermis. These cells contain organelles called melanosomes, which synthesize melanin through a complex enzymatic process involving tyrosinase, the key enzyme in melanin production.
Under normal circumstances, melanocytes distribute melanin evenly throughout the skin, creating our natural skin tone. However, various factors can disrupt this delicate balance, causing melanocytes to become hyperactive in certain areas, leading to hyperpigmentation disorders like melasma.
The melanin production process involves two main types of melanin: eumelanin (brown-black pigment) and pheomelanin (red-yellow pigment). The ratio and concentration of these pigments determine individual skin color and how the skin responds to various triggers. In melasma, there’s typically an overproduction of eumelanin in affected areas, creating the characteristic dark patches (Sheth & Pandya, 2011, Journal of the American Academy of Dermatology).

What is Melasma? A Detailed Overview
Melasma is a chronic, acquired hypermelanosis characterized by symmetric brown or gray-brown patches on sun-exposed areas of the face. It affects approximately 10-15% of pregnant women and up to 5 million Americans annually, with women of reproductive age being disproportionately affected, comprising 90% of all cases (Handel et al., 2014, American Journal of Clinical Dermatology).
The condition manifests in three distinct patterns: centrofacial (covering the cheeks, forehead, upper lip, nose, and chin), malar (affecting the cheeks and nose), and mandibular (appearing along the jawline). The centrofacial pattern is the most common, accounting for approximately 65% of cases.
Melasma patches are typically bilateral and symmetric, though unilateral presentation can occur. The pigmentation can vary from light brown to dark brown or even blue-gray, depending on the depth of melanin deposition in the skin layers. Epidermal melasma appears brown and responds better to treatment, while dermal melasma appears blue-gray and proves more challenging to treat. Mixed melasma, containing both epidermal and dermal components, is the most common type.
The Complex Web of Melasma Causes
Hormonal Influences: The Primary Driver
Hormonal fluctuations represent the most significant contributing factor to melasma development. Estrogen and progesterone, particularly when elevated during pregnancy, oral contraceptive use, or hormone replacement therapy, directly stimulate melanocyte activity. These hormones increase the expression of melanogenic proteins and enhance the skin’s sensitivity to other melasma triggers.
During pregnancy, rising estrogen levels can increase by 1000-fold, while progesterone levels increase significantly throughout gestation. This dramatic hormonal surge explains why melasma affects 15-50% of pregnant women, earning it the nickname “pregnancy mask.” The condition often appears during the second or third trimester and may fade postpartum, though complete resolution isn’t guaranteed (Ogbechie-Godec & Elbuluk, 2017, American Journal of Clinical Dermatology).
Oral contraceptives containing both estrogen and progestin can trigger melasma in susceptible individuals. Studies show that 8-29% of women using combined oral contraceptives develop melasma, with the risk being highest in the first few months of use (Trivedi et al., 2017, Indian Dermatology Online Journal). Hormone replacement therapy during menopause can also precipitate melasma development, particularly in women with a history of pregnancy-related melasma.
Solar Radiation: The Amplifying Factor
Ultraviolet (UV) radiation acts as a powerful trigger and exacerbating factor for melasma. Both UVA (320-400nm) and UVB (290-320nm) radiation stimulate melanocyte activity, but UVA penetrates deeper into the skin and plays a more significant role in melasma development and persistence.
UV exposure triggers a cascade of cellular events leading to increased melanin production. It activates transcription factors like microphthalmia-associated transcription factor (MITF), which regulates genes involved in melanocyte proliferation and melanin synthesis. Additionally, UV radiation generates reactive oxygen species (ROS) that can damage DNA and trigger inflammatory responses, further stimulating melanogenesis.
Visible light (400-700nm) and infrared radiation (700nm-1mm) also contribute to melasma development and should not be overlooked. Recent research suggests that visible light, particularly blue light from digital devices, can stimulate melanin production in darker skin types, making comprehensive photoprotection essential (Mahmoud et al., 2010, Photochemistry and Photobiology).
Genetic Predisposition: The Foundation Factor
Genetic factors significantly influence melasma susceptibility and severity. Studies indicate that 33-50% of melasma patients have a family history of the condition, suggesting a strong hereditary component. Certain genetic polymorphisms affect how individuals respond to hormonal fluctuations and UV exposure.
Variations in genes encoding melanogenic enzymes, such as tyrosinase, tyrosinase-related protein 1 (TRP-1), and dopachrome tautomerase (DCT), can influence melanin production capacity. Additionally, polymorphisms in genes regulating hormone metabolism and UV response pathways may predispose individuals to melasma development.
Ethnicity plays a crucial role, with melasma being more prevalent in individuals with darker skin types (Fitzpatrick skin types III-V). Hispanic, Asian, and Middle Eastern populations show higher melasma incidence rates, likely due to genetic factors combined with geographic and cultural sun exposure patterns.
Environmental and Lifestyle Factors
Beyond the primary triggers, numerous environmental and lifestyle factors can contribute to melasma development and persistence:
Heat Exposure: High temperatures and heat-generating activities can worsen melasma by increasing blood flow to facial skin and potentially stimulating melanocyte activity. This includes exposure to cooking heat, saunas, hot yoga, and even heated car interiors.
Cosmetic Products: Certain skincare ingredients can increase photosensitivity or cause irritation that triggers post-inflammatory hyperpigmentation. Fragrances, essential oils, and some active ingredients like retinoids (when used incorrectly) can exacerbate melasma.
Medications: Various medications can increase photosensitivity and melasma risk, including certain antibiotics, anti-seizure medications, and antimalarial drugs. Phototoxic and photoallergic reactions from medications can worsen existing melasma or trigger new patches.
Stress: Chronic stress elevates cortisol levels, which can indirectly affect hormone balance and inflammation, potentially contributing to melasma development or persistence.

Current Treatment Landscape: What Works and What Doesn’t
Topical Treatments: The First Line of Defense
Hydroquinone: Considered the gold standard for melasma treatment, hydroquinone inhibits tyrosinase enzyme activity, reducing melanin production. Available in 2% over-the-counter formulations and 4% prescription strengths, hydroquinone can be effective but requires careful monitoring due to potential side effects like ochronosis (blue-black pigmentation) with prolonged use.
Tretinoin: This vitamin A derivative accelerates skin cell turnover and helps disperse existing melanin. When combined with hydroquinone, tretinoin enhances penetration and efficacy. However, it can cause initial irritation and increased photosensitivity.
Corticosteroids: Mild topical steroids like fluocinolone acetonide help reduce inflammation and can enhance the effectiveness of other lightening agents. They’re typically used in combination formulations rather than as monotherapy.
Triple Combination Therapy: The most effective topical approach combines hydroquinone, tretinoin, and a mild corticosteroid. This combination addresses multiple aspects of melasma pathophysiology but requires careful monitoring and gradual introduction to minimize irritation.
Alternative Topical Agents: For those who cannot tolerate hydroquinone, alternatives include kojic acid, arbutin, vitamin C, azelaic acid, and licorice extract. While generally gentler, these agents may be less effective and require longer treatment periods.
Professional Procedures: Advanced Interventions
Chemical Peels: Superficial peels using glycolic acid, lactic acid, or salicylic acid can help remove superficial pigmentation and enhance topical treatment penetration. Medium-depth peels may be considered for resistant cases but carry higher risks of post-inflammatory hyperpigmentation.
Laser Therapy: Various laser systems have been used for melasma with mixed results. Q-switched lasers, fractional lasers, and picosecond lasers can target melanin deposits, but they also carry risks of worsening pigmentation, particularly in darker skin types.
Microneedling: This procedure creates controlled micro-injuries to stimulate skin renewal and enhance topical product penetration. When combined with appropriate serums, microneedling can improve melasma appearance with minimal downtime.
Intense Pulsed Light (IPL): IPL targets melanin using broad-spectrum light but has shown inconsistent results for melasma and may worsen the condition in some patients.
Limitations and Challenges of Conventional Treatments
Despite numerous available treatments, melasma remains notoriously difficult to treat completely. Many conventional approaches focus solely on melanin reduction without addressing underlying hormonal and inflammatory factors. This narrow approach often leads to temporary improvements followed by recurrence.
Side effects represent another significant limitation. Hydroquinone can cause contact dermatitis, rebound hyperpigmentation, and, rarely, ochronosis. Tretinoin frequently causes initial irritation, dryness, and increased sun sensitivity. Laser treatments carry risks of burns, scarring, and paradoxical hyperpigmentation.
The chronic, recurrent nature of melasma means that most treatments require long-term maintenance, which can be costly and time-consuming. Many patients experience frustration with the slow pace of improvement and the need for ongoing treatment to maintain results.

The Power of Natural and Ayurvedic Approaches
While conventional treatments focus primarily on suppressing melanin production, traditional medicine systems like Ayurveda take a more holistic approach, addressing the root causes of skin discoloration while supporting overall skin health and balance.
Understanding Ayurvedic Principles for Skin Health
In Ayurveda, skin health is intrinsically linked to overall constitutional balance and the harmony of the three doshas: Vata (air and space), Pitta (fire and water), and Kapha (earth and water). Melasma and hyperpigmentation are often attributed to Pitta imbalance, characterized by excess heat and inflammation in the body.
Ayurvedic treatment approaches focus on cooling and balancing Pitta dosha while supporting the body’s natural detoxification processes. This involves both internal purification and external treatments using carefully selected herbs and natural ingredients that have been used for centuries to promote clear, radiant skin.
Key Ayurvedic Ingredients for Pigmentation
Turmeric (Curcuma longa): Known as “Haridra” in Sanskrit, turmeric contains curcumin, a powerful anti-inflammatory and antioxidant compound. Research shows curcumin can inhibit tyrosinase activity, reduce melanin production, and protect against UV-induced skin damage. Its anti-inflammatory properties help calm irritated skin and prevent post-inflammatory hyperpigmentation.
Saffron (Crocus sativus): Considered one of the most precious ingredients in Ayurveda, saffron contains compounds like crocin and crocetin that possess potent antioxidant and skin-lightening properties. Studies demonstrate saffron’s ability to inhibit melanogenesis and protect against UV damage while promoting skin radiance and even tone.
Multani Mitti (Fuller’s Earth): This natural clay has been used for centuries to purify and brighten skin. Rich in minerals like magnesium, aluminum, and silica, Multani Mitti gently exfoliates dead skin cells, absorbs excess oil, and helps fade dark spots and hyperpigmentation.
Fenugreek (Trigonella foenum-graecum): Known as “Methi” in Hindi, fenugreek seeds contain compounds that help brighten skin and reduce pigmentation. The seeds are rich in vitamins, minerals, and antioxidants that nourish skin while supporting natural cell turnover.
Wild Turmeric (Curcuma aromatica): Distinct from common turmeric, wild turmeric or “Kasturi Haldi” is specifically prized for cosmetic applications. It provides the benefits of regular turmeric without staining the skin and is particularly effective for treating hyperpigmentation and uneven skin tone.
Vitamin E: A powerful antioxidant that protects skin from free radical damage and supports healing. Vitamin E helps maintain skin barrier function and can enhance the absorption and effectiveness of other active ingredients.
Aloe Vera: Renowned for its soothing and healing properties, aloe vera contains compounds that can inhibit tyrosinase activity and reduce melanin production. Its anti-inflammatory effects help calm irritated skin and support the healing process.
The Science Behind Natural Pigmentation Solutions
Modern research increasingly validates traditional knowledge about natural ingredients for treating hyperpigmentation. Many plant compounds work through multiple mechanisms to address different aspects of melasma:
Tyrosinase Inhibition: Many natural compounds, including those found in licorice root, kojic acid (from fungi), and various plant extracts, can inhibit tyrosinase enzyme activity, reducing melanin production at its source.
Antioxidant Protection: Natural antioxidants neutralize free radicals that can trigger melanocyte activation and inflammation. This protective effect is crucial for preventing further pigmentation and supporting skin repair.
Anti-inflammatory Action: Chronic inflammation contributes to melasma persistence and can trigger post-inflammatory hyperpigmentation. Natural anti-inflammatory compounds help break this cycle and promote healing.
Gentle Exfoliation: Natural fruit acids and enzymes provide gentle exfoliation that helps remove pigmented skin cells and promote cell turnover without the harsh side effects of synthetic alternatives.
Introducing Vishada Pinja: A Traditional Solution for Modern Skin Concerns
Drawing from 70 years of traditional formulation expertise, Daadipharma has developed Vishada Pinja Ayurvedic Pigmentation and Melasma Cream, a comprehensive natural solution that addresses the complex nature of skin pigmentation disorders. This carefully crafted formulation combines time-tested Ayurvedic ingredients with modern understanding of skin science to provide effective, gentle treatment for melasma and hyperpigmentation.
The Science-Backed Formulation
Vishada Pinja represents the culmination of seven decades of research and refinement in traditional medicine. Each 30g tube contains a precise blend of premium ingredients selected for their synergistic effects on skin pigmentation:
Lentil Extract: Rich in natural enzymes and proteins that gently exfoliate and brighten skin while providing essential nutrients for healthy cell turnover.
Saffron Extract: Concentrated saffron provides potent antioxidant protection and melanin-inhibiting compounds that help fade existing pigmentation while preventing new spots from forming.
Multani Mitti: This mineral-rich clay purifies pores, absorbs excess oil, and provides gentle physical exfoliation to reveal brighter, more even-toned skin beneath.
Fenugreek Seed Extract: Delivers vitamins, minerals, and brightening compounds that support natural skin renewal and help reduce the appearance of dark spots and uneven pigmentation.
Wild Turmeric: Provides all the anti-inflammatory and brightening benefits of regular turmeric without the risk of yellow staining, making it ideal for facial application.
Vitamin E: Protects against environmental damage while supporting skin barrier function and enhancing the stability and effectiveness of other active ingredients.
Aloe Vera: Soothes irritation, provides hydration, and contributes additional melanin-inhibiting compounds while supporting the skin’s natural healing processes.
A Holistic Approach to Pigmentation Treatment
Unlike conventional treatments that focus solely on melanin suppression, Vishada Pinja addresses multiple factors contributing to melasma and hyperpigmentation:
Comprehensive Melanin Management: The formulation works through multiple pathways to reduce melanin production, including tyrosinase inhibition, antioxidant protection, and anti-inflammatory action.
Skin Barrier Support: Natural moisturizing and barrier-supporting ingredients help maintain healthy skin function, which is essential for preventing irritation-induced hyperpigmentation.
Gentle Yet Effective: The natural formulation provides effective results without the harsh side effects commonly associated with synthetic lightening agents.
Long-term Safety: With ingredients used safely for centuries, Vishada Pinja offers a sustainable long-term approach to pigmentation management.
Clinical Benefits and Expected Results
Users of Vishada Pinja can expect to see gradual improvement in their skin’s appearance with consistent use:
Week 1-2: Initial benefits include improved skin texture, reduced irritation, and enhanced radiance as the natural ingredients begin their work.
Week 3-4: Subtle lightening of pigmented areas may become apparent as melanin production begins to normalize and gentle exfoliation reveals fresher skin.
Month 2: More noticeable improvement in pigmentation intensity and overall skin tone evenness as the cumulative effects of the natural ingredients build.
Month 3 and Beyond: Significant improvement in melasma and hyperpigmentation with continued use, as recommended for optimal results.
The gradual, natural approach ensures sustainable results without the rebound effects often seen with harsher treatments.
Proper Application and Usage Guidelines
To maximize the benefits of Vishada Pinja, proper application is essential:
Step 1: Cleanse the affected area thoroughly with a gentle cleanser and pat dry.
Step 2: Apply 3 drops of the cream to the affected areas, using gentle circular motions to ensure even distribution.
Step 3: Rinse with water in the morning after overnight application, or leave on for the recommended duration for day use.
Step 4: Apply a broad-spectrum sunscreen if using during the day, as consistent sun protection is crucial for preventing further pigmentation.
The cream should be used consistently for at least 3 months to achieve optimal results, as natural ingredients work gradually to restore skin balance and reduce pigmentation.
Safety Profile and Suitable Candidates
Vishada Pinja is formulated to be safe for long-term use in men and women aged 15 and above. The natural ingredient profile minimizes the risk of adverse reactions commonly associated with synthetic lightening agents.
The cream is particularly suitable for:
- Individuals with pregnancy-related melasma
- Those seeking natural alternatives to conventional treatments
- People with sensitive skin who cannot tolerate harsh chemicals
- Anyone looking for a sustainable, long-term approach to pigmentation management

Prevention Strategies: Protecting Your Investment in Clear Skin
While treating existing melasma is important, prevention remains the most effective long-term strategy. Implementing comprehensive prevention measures can help maintain treatment results and prevent new pigmentation from developing.
Sun Protection: The Non-Negotiable Foundation
Rigorous sun protection forms the cornerstone of melasma prevention and management. This includes:
Broad-Spectrum Sunscreen: Use SPF 30 or higher daily, reapplying every 2 hours and after swimming or sweating. Look for formulations containing zinc oxide or titanium dioxide for physical protection.
Protective Clothing: Wide-brimmed hats, long sleeves, and UV-protective clothing provide additional protection, especially during peak sun hours.
Seek Shade: Limit direct sun exposure, particularly between 10 AM and 4 PM when UV radiation is strongest.
Window Protection: UV rays can penetrate glass, so consider UV-protective window films for cars and homes.
Lifestyle Modifications
Heat Avoidance: Minimize exposure to excessive heat from cooking, saunas, or hot environments that can trigger melasma flare-ups.
Gentle Skincare: Use mild, fragrance-free products to avoid irritation that can trigger post-inflammatory hyperpigmentation.
Stress Management: Practice stress-reduction techniques like meditation, yoga, or regular exercise to help maintain hormonal balance.
Hormonal Considerations: Discuss melasma risk with healthcare providers when considering hormonal contraceptives or hormone replacement therapy.

The Future of Natural Pigmentation Treatment
As research continues to validate traditional knowledge about natural ingredients for skin health, the future of pigmentation treatment is likely to embrace more holistic approaches that combine the best of both traditional wisdom and modern science.
Emerging research on the skin microbiome, circadian rhythms, and the gut-skin axis suggests that effective melasma treatment may require addressing multiple body systems simultaneously – an approach that aligns closely with traditional Ayurvedic principles.
Recap: Embracing a Holistic Path to Clear, Radiant Skin
Melasma and hyperpigmentation represent complex conditions that require comprehensive, patient approaches to treatment. While conventional therapies focus primarily on suppressing melanin production, natural and Ayurvedic approaches like Vishada Pinja offer a more balanced solution that addresses multiple contributing factors while supporting overall skin health.
The journey to clearer, more even-toned skin requires patience, consistency, and the right combination of treatments and prevention strategies. By choosing natural solutions backed by centuries of traditional knowledge and modern research, individuals can achieve lasting improvements in their skin’s appearance while avoiding the harsh side effects often associated with synthetic alternatives.
Vishada Pinja Ayurvedic Pigmentation and Melasma Cream represents more than just another skincare product – it embodies a holistic philosophy that recognizes the interconnected nature of skin health and overall well-being. With its carefully selected ingredients, proven safety profile, and comprehensive approach to pigmentation management, Vishada Pinja offers hope and effective treatment for those seeking natural solutions to their skin concerns.
Remember, achieving optimal results requires patience and consistency. The skin’s natural renewal cycle takes time, and lasting improvements develop gradually. By embracing a natural approach with Vishada Pinja and implementing comprehensive prevention strategies, you can work toward the clear, radiant skin you deserve while supporting your skin’s long-term health and resilience.
For those ready to embark on a natural journey toward clearer skin, Vishada Pinja offers a time-tested, scientifically-informed solution that honors both traditional wisdom and modern understanding of skin health. Your path to more confident, radiant skin begins with making the choice to treat your skin with the gentle, effective care it deserves.
References
- Sheth, V.M. & Pandya, A.G. (2011). Melasma: a comprehensive update: part I. Journal of the American Academy of Dermatology
- Handel, A.C., Miot, L.D., & Miot, H.A. (2014). Melasma: a clinical and epidemiological review. Anais Brasileiros de Dermatologia
- Ogbechie-Godec, O.A. & Elbuluk, N. (2017). Melasma: an Up-to-Date Comprehensive Review. Dermatology and Therapy
- Trivedi, M.K., Yang, F.C., & Cho, B.K. (2017). A review of laser and light therapy in melasma. Indian Dermatology Online Journal
- Mahmoud, B.H., Hexsel, C.L., Hamzavi, I.H., & Lim, H.W. (2010). Effects of visible light on the skin. Photochemistry and Photobiology
- Tamega et al. (2013) – Anais Brasileiros de Dermatologia
- Zhai & Maibach (2004) – Skin Research and Technology